https://emedicine.medscape.com/article/281237-overview
Rectal cancer is a disease in which cancer cells form in the tissues of the rectum; colorectal cancer occurs in the colon or rectum. Adenocarcinomas comprise the vast majority (98%) of colon and rectal cancers; more rare rectal cancers include lymphoma (1.3%), carcinoid (0.4%), and sarcoma (0.3%).
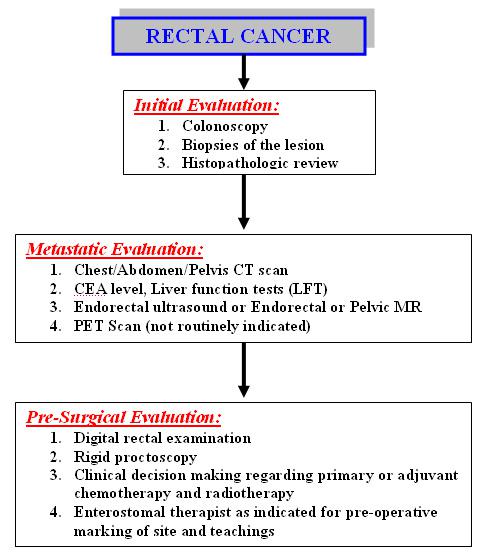
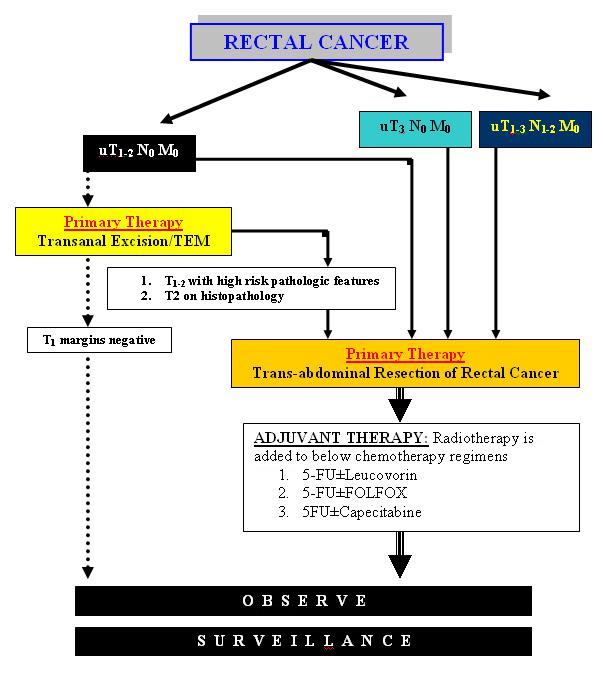
The incidence and epidemiology, etiology, pathogenesis, and screening recommendations are common to both colon cancer and rectal cancer. The image below depicts the staging and workup of rectal cancer.
Diagnostics. Staging and workup of rectal cancer patients.
Signs and symptoms
Bleeding is the most common symptom of rectal cancer, occurring in 60% of patients. However, many rectal cancers produce no symptoms and are discovered during digital or proctoscopic screening examinations.
Other signs and symptoms of rectal cancer may include the following:
Change in bowel habits (43%): Often in the form of diarrhea; the caliber of the stool may change; there may be a feeling of incomplete evacuation and tenesmus
Occult bleeding (26%): Detected via a fecal occult blood test (FOBT)
Abdominal pain (20%): May be colicky and accompanied by bloating
Back pain: Usually a late sign caused by a tumor invading or compressing nerve trunks
Urinary symptoms: May occur if a tumor invades or compresses the bladder or prostate
Malaise (9%)
Pelvic pain (5%): Late symptom, usually indicating nerve trunk involvement
Emergencies such as peritonitis from perforation (3%) or jaundice, which may occur with liver metastases (< 1%)
See Clinical Presentation for more detail.
Diagnosis
Perform physical examination with specific attention to the size and location of the rectal tumor in addition to possible metastatic lesions, including enlarged lymph nodes or hepatomegaly. In addition, evaluate the remainder of the colon.
Examination includes the use of the following:
Digital rectal examination (DRE): The average finger can reach approximately 8 cm above the dentate line; rectal tumors can be assessed for size, ulceration, and presence of any pararectal lymph nodes, as well as fixation to surrounding structures (eg, sphincters, prostate, vagina, coccyx and sacrum); sphincter function can be assessed
Rigid proctoscopy: This examination helps to identify the exact location of the tumor in relation to the sphincter mechanism
Laboratory tests
Routine laboratory studies in patients with suspected rectal cancer include the following:
Complete blood count
Serum chemistries
Liver and renal function tests
Carcinoembryonic antigen (CEA) test
Histologic examination of tissue specimens
Screening tests may include the following:
Guaiac-based FOBT
Stool DNA screening (SDNA)
Fecal immunochemical test (FIT)
Rigid proctoscopy
Flexible sigmoidoscopy (FSIG)
Combined glucose-based FOBT and flexible sigmoidoscopy
Double-contrast barium enema (DCBE)
Computed tomography (CT) colonography
Fiberoptic flexible colonoscopy (FFC)
Imaging studies
If metastatic (local or systemic) rectal cancer is suspected, the following radiologic studies may be obtained:
CT scanning of the chest, abdomen, and pelvis
Endorectal ultrasonography
Endorectal or pelvic magnetic resonance imaging (MRI)
Positron emission tomography (PET) scanning: Not routinely indicated
See Workup for more detail.
Management
A multidisciplinary approach that includes colorectal surgery/surgical oncology, medical oncology, and radiation oncology is required for optimal treatment of patients with rectal cancer. Surgical technique, use of radiotherapy, and method of administering chemotherapy are important factors.
Strong considerations should be given to the intent of surgery, possible functional outcome, and preservation of anal continence and genitourinary functions. The first step involves achievement of cure, because the risk of pelvic recurrence is high in patients with rectal cancer, and locally recurrent rectal cancer has a poor prognosis.
Surgery
Radical resection of the rectum is the mainstay of therapy. The timing of surgical resection is dependent on the size, location, extent, and grade of the rectal carcinoma. Operative management of rectal cancer may include the following:
Transanal excision: For early-stage cancers in a select group of patients
Transanal endoscopic microsurgery: Form of local excision that uses a special operating proctoscope that distends the rectum with insufflated carbon dioxide and allows the passage of dissecting instruments
Endocavity radiotherapy: Delivered under sedation via a special proctoscope in the operating room
Sphincter-sparing procedures: Low anterior resection, coloanal anastomosis, abdominal perineal resection
Adjuvant medical management
Adjuvant medical therapy may include the following:
Adjuvant radiation therapy
Intraoperative radiation therapy
Adjuvant chemotherapy
Adjuvant chemoradiation therapy
Radioembolization
Pharmacotherapy
The National Comprehensive Cancer Network guidelines recommend the use of as many chemotherapy drugs as possible to maximize the effect of adjuvant therapies for colon and rectal cancer.
The following agents may be used in the management of rectal cancer:
Antineoplastic agents (eg, fluorouracil, vincristine, leucovorin, irinotecan, oxaliplatin, cetuximab, bevacizumab, panitumumab)
Vaccines (eg, quadrivalent human papillomavirus [HPV] vaccine)